By Donna Hoffmeyer
(original post on Medium)
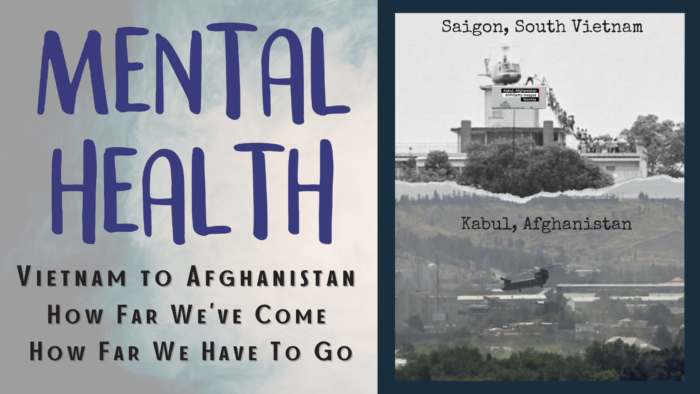
The fall of Saigon and the fall of Afghanistan. Similar scenarios, same fear.
It got me thinking about the trauma the people, military and civilian, have experienced and are still currently experiencing; and the wide disparity of mental healthcare available during Vietnam (and earlier) versus today.
I flashed back to when I was a child. My great Uncle Joe was a quiet guy; hardly said a word..unless he was drinking. He was probably considered a pretty severe alcoholic. I say probably, as I was a kid and only knew he was considered a drunk by various family members. I didn’t know much about him until my brother had a report to do on Normandy. He asked Uncle Joe if he could interview him. Ah, the power of innocence. This was the only time anyone ever heard him speak about his time in the military.
Uncle Joe was a war hero. Remember the cliff scene in Private Ryan? That was Uncle Joe. He was one of the “lucky” ones that survived Normandy. As a child, I was enthralled hearing his story but never connected the dots to his alcohol abuse. As an adult, my heart broke knowing he re-lived that day every day until he passed away in his 80s.
After my Pop returned from WWII, he developed a significant startle reflex. It was known you did not jump out and scare him, nor did you volunteer to wake him from a deep sleep. Both instances would put you at risk of getting involuntarily decked. He held that reflex until the day he passed away.
When I had the opportunity to watch a neuropsychological evaluation years ago, I listened as a Vietnam Veteran told the psychiatrist how he dove behind the recliner he slept in when he was startled awake by a thunderstorm. He had no idea he was dealing with PTSD.
Of the three scenarios, only one received any mental health care…30 years later.
Nearly 2-years ago, the military and veteran community was mentally rocked by the disjointed pull-out and rapid takeover of Afghanistan by the Taliban. What stood out to me immediately, was the number of entities that ramped up mental health resources. VA, nonprofits, DoD, other veterans…social media was flooded with resources and people were sharing these resources over and over. It was truly amazing to watch the outpouring of help.
Between the picture and the expansion of available mental health resources, I thought about how far we have come since Vietnam. The war where soldiers came home and were shunned, had their backs turned on them, and had little to no resources to help them process their mental and moral injuries. They became recluses, hermits, and stoics…never talked about it. They drank to cope, and instead of receiving help, they were labeled as drunks. They were put aside for years.
Today, mental health is slowly starting to lose its stigma. We are beginning to see strength in asking for help. Commanders and other leaders are learning what it means to be constructively vulnerable and understanding the benefits of being vulnerable — not only as an example for their subordinates, but for their psyche as well. Peers are offering a hand, instead of turning back. This is collectively reinforced by the civilian world — actors, sports figures, and singers are all stepping forward and owning their mental health. Yes, I realize they may not be the first people Veterans look to for internal validation…but they provide consistency in the message.
However, do not fall under the fallacy we have arrived. We are far far far from it…we are just starting. Yes, the Me Too movement brought enormous light to sexual assault, but the military still has a problem handling it. Yes, there are more entities offering service, but quantity (which is still constrained) is far exceeding quality. In defense, the greater the need, the more we are tapping these finite resources and burning out the good ones…leaving us with mediocre care at best, and in reality, not improving outcomes.
I say this, having helped many with military mental health care, as well as navigating the system myself. I’ve heard the stories, watched the disasters, and experienced my own frustrations. When you walk in for talk therapy and are told by the military psychiatrist, she can only help you if you want medication, otherwise it is a 3-month wait for a mental health appointment, there is a serious problem. (True story.)
The civilian side is not much better. Our son has ADHD and we were told that the clinic he goes to, cannot manage his medication anymore. All the providers left and they cancelled all medication appointments for the rest of the year.
I received a call from a close friend, desperate for care for chronic bulimia, as a result of years of domestic and sexual abuse both in and out of the military. Her VA provider, psychiatrist, and therapist all agreed inpatient was her best option. However, they were not the final approval. The Chief of Mental Health at her VA would not allow her to get inpatient care…he has never laid eyes on her.
I could go on with story after story. The bottom line is we need to level up mental health care — quality, quantity, and coverage. We need to invest in producing quality mental health providers and figuring out how to better match providers and patients. We need more therapists that are truly invested in their patient’s well-being, and mental health case managers to help navigate the confusing and often disjointed system. While we are at it, let’s smooth out the system. DoD needs to bring on more civilian providers with military backgrounds. There is nothing worse than having someone that does not even understand military culture. There needs to be more communication, collaboration, and fluidity between military, civilian, and VA care. Rather than rationing mental health care, insurances need better communication with facilities to re-evaluate at specified periods and determine the best course of action for the patient…not their pocketbooks. How hard is it to understand earlier intervention leads to better outcomes for the patient and cost savings for insurance? Stop being stingy.
To our veterans from Vietnam and earlier, thank you for your service and perseverance. Your struggles were the machetes that have hacked, dug, and carved out the path we have today. It’s still bumpy, but at least there is a path where before there was none.
To all our veterans and soon-to-be veterans, please do not give up. You gave everything! You are here for a purpose. You are worthy and deserving of quality care. Keep fighting for it.
Yes, mental health care has made leaps and bounds from our early wars, however, the surface has only been scratched. Both military and civilian communities are working toward normalizing mental health issues.
Awesome.
Now who is going to give quality care to all these people now brave enough to seek services? Commanders and leaders, are you fighting for early intervention to retain your highly trained assets? Providers, are you hearing your patients/caregivers? Insurance, are you covering what is truly needed vice what the algorithm tells you is needed? No, we have not arrived, not even close.
However, I remain hopeful we are moving in the right direction.